The Knee Joint
Learn more about the anatomy and damage of a knee joint, the fixation of an artificial knee joint and what happens before the surgery.
Anatomy: How is the Knee Joint Structured?
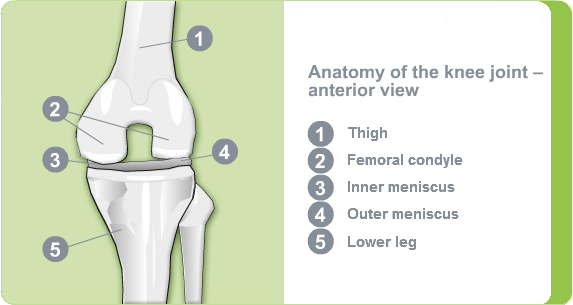
The knee joint essentially consists of three bone parts:
- Thighbone (femur)
- Shinbone (tibia)
- Kneecap (patella)
On the joint surface of the thighbone, there are two bony protrusions, which are referred to as condyles. The joint surface of the shinbone is referred to as the tibial plateau. When in a healthy condition, both joint surfaces are covered with a layer of joint cartilage, that acts as a kind of shock absorber. The synovial fluid acts as a lubricant and enables smooth movements of the bones and reduces friction.
The menisci sit between the thighbone and the shinbone. The two menisci, medial and lateral, are crescent-shaped and consist of fibrocartilage. They enable force to be better distributed in the knee, thus protecting the cartilage-covered joint surfaces.
The kneecap is embedded in the tendon structure which extends from the thighbone to the shinbone. When the leg is stretched and flexed, the kneecap slides up or down thus stabilising the knee joint at the front.
Role of the Joint Capsule
The knee joint is surrounded by a fixed articular capsule, which seals it off from the surrounding tissue. The articular capsule produces synovial fluid, which supplies the cartilage with nutrients and helps the knee joint to move free from friction.
Stability and Movement Thanks to Ligaments and Muscles
The knee joint is stabilised by a complex set of ligaments:
The collateral ligaments hold the joint in place on the inside and outside, while the cruciate ligaments stabilise the front and rear of the knee joint. This means the knee is a very stable joint despite being subject to considerable forces, whereby the powerful leg movements are supported by strong muscles.
Damage of the Knee Joint - What is Knee Arthrosis?
If the protective layer of joint cartilage becomes worn or damaged, this is referred to as knee arthrosis.
This can be due to a number of causes:
- wear of the joint cartilage for unexplained reasons (idiopathic arthrosis)
- inflammation of the joint (chronic arthritis, rheumatism)
- hereditary knee joint dysplasia (knock knee or bow leg)
- incorrect loading or overloading of the knee joint during work or sporting activities; accidents with knee involvement
- excess weight is regarded as an adverse factor in the development and progression of gonarthrosis
In a healthy knee joint, the joint cartilage forms a smooth surface and the menisci protect the joint surfaces against friction.
In the case of knee arthrosis, damage is often first caused to the cartilaginous menisci, which can then no longer sufficiently protect the joint surfaces against pressure exerted by the weight of the body.
Over time, the joint surfaces of the femoral condyle and the tibial plateau are then also affected: the protective coating of cartilage becomes roughened at the points where the load is greatest and over the course of time wears away entirely.

Pain and Restricted Movement
If the joint surfaces rub against each other without a protective layer of cartilage, the person affected experiences pain. At first, the patient only experiences pain when the joint is under stress, yet over time, pain is increasingly experienced when at rest, particularly at night. The pain mainly occurs in the area of the affected knee, but can also radiate out to the thigh or the buttocks.
The knee joint also increasingly loses its mobility, until it becomes completely stiff. As a result of this, patients adopt a protective posture, which in turn causes muscle tension and pain in other areas of the body, such as the hips and back.
As the knee joint plays a key role in day-to-day activities, patients become increasingly restricted in their everyday life and their quality of life can diminish. Even getting out of bed or a chair, climbing the stairs or getting into and out of a car can become a challenge.
Pain Relief Options
Depending on the nature of the pain experienced, the attending doctor will firstly try conservative methods to ease the pain. These include pain relief and anti-inflammatory medication, physiotherapy, baths and packs. These help to reduce the pain and improve joint mobility. Knee arthroscopy with irrigation of the articular cavity can also bring temporary relief.
However, there is currently no sure way of recreating an intact cartilage layer in the joint and healing arthrosis. Thus, if all the measures fail to ease the pain, patients can be helped with a replacement of the diseased joint using a knee endoprosthesis.
Artificial Knee Joint - The Artificial Knee Replacement
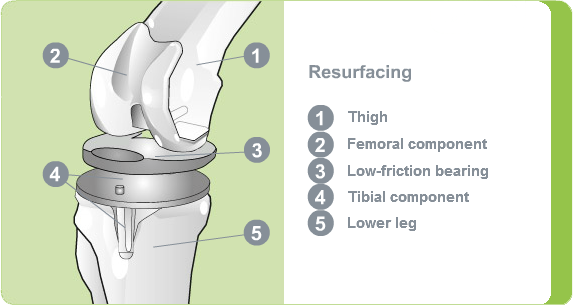
An artificial knee joint consists of the following parts, e.g.:
- metal alloys (cobalt-chromium molybdenum metal alloys due to good tolerability and durability)
- special plastic polymers (replicate the layer of cartilage covering the joint)
The surgeon will decide which materials will be suitable for each individual patient.
In many cases it is sufficient just to replace the damaged structures close to the knee joint. This involves fitting a femur joint replacement to the condyle and a tibial plateau replacement to the shinbone. A plastic insert acts as a low-friction bearing between the two. The back of the kneecap can also be replaced with a plastic cap.
This procedure is referred to as resurfacing as only the damaged surfaces are replaced. One benefit of this intervention is that the bone material is preserved and the important, supportive tendon structures are retained as much as possible. For this reason, this procedure is currently the standard knee replacement operation.
Fixation Artificial Knee Joint - How is the Knee Prosthesis Fixated?
An artificial knee joint can be fixated in a variety of ways. In essence, there are two main types of fixation: cemented and cementless:
- If the bone structure lacks stability, the knee joint replacement is fixated using bone cement. This creates a strong bond between the knee endoprosthesis and the bone immediately after the surgery.
- If the bone quality is good, the artificial knee joint can be fixated without using cement. In this case, the bone slowly grows into the knee endoprosthesis and it takes some time to create a strong connection.
The correct choice of procedure not only depends on the age and physical activity of the patient, but also on the condition of the bone. The surgeon decides on the appropriate method with the patient during a preoperative consultation.
With this method, the artificial femoral and tibial components are bonded to the bone using bone cement. Bone cement is always used when the back of the kneecap is replaced.
What Happens Before Surgery?
Patient Assessment – Your Personal Medical History
In the initial consultation the doctor will ask you about your complaints. They will ask where you have pain and where this pain radiates to. They will also enquire about the intensity of the pain, how long it lasts and any influencing factors which exacerbate or ease the pain.
Physical Examination – Where Does it Hurt?
The doctor will first examine your knee, pelvis, hips and spine, and palpate the various muscle and bone structures. They will then conduct some movement tests to gain an impression of the mobility of the knee joint. They will also check the level of pain caused by various movements in the knee joint, such as rotation, bending and stretching.
X-ray – Focus on Your Knee
Using an X-ray image, the doctor is able to identify changes caused by knee arthrosis: Owing to a loss of cartilage, the intra-articular space between the femoral condyle and the tibial plateau is either no longer uniform, is narrower or is even no longer visible. The bone structure of the femoral condyle and tibial plateau, and in some cases the kneecap, appears irregular and altered; in very advanced stages the sections of the joint are deformed.
Preoperative Discussion – Your Chance to Ask any Questions
On the day before surgery, the surgeon will usually discuss the procedure with you in detail. During the consultation, they will explain the surgical method and the type of prosthesis to be used. Selecting the right prosthesis model depends on your individual bone condition, your body weight and your physical activity. The surgeon therefore normally decides beforehand which prosthesis model and type of fixation to use based on your X-ray and data.
On the day of the surgery, it is important that you are in a good general state of health. In light of this, it is important that you discuss any complaints you have with the attending doctor, whether it is a cold or a skin infection. While these conditions are harmless, they must be cured before a surgical intervention, in order to minimise any further risks.
An anaesthetist will also talk to you on the day before the operation to explain the potential risks involved with the anaesthesia. They will also perform a few minor examinations to check your heart and lung functions and rule out any possible allergies. They will then talk to you about the type of anaesthesia to be used.
Autologous Blood Donations – Find out More!
Under certain circumstances, a knee prosthesis surgery may result in considerable blood loss. In this event, a blood transfusion will then be required. An autologous blood transfusion using the patient's own blood, donated at an earlier date, essentially rules out the risk of infections such as Hepatitis C and HIV. There is normally enough time between the diagnosis and the knee prosthesis surgery (around two to six weeks) to discuss this issue with your attending doctor. Use this opportunity to ask about the option of an autologous blood donation.


