The Shoulder Joint
Learn more about the anatomy and damage of a shoulder joint, the fixation of an artificial shoulder joint and what happens before the surgery.
Anatomy: How is the Shoulder Joint Structured?
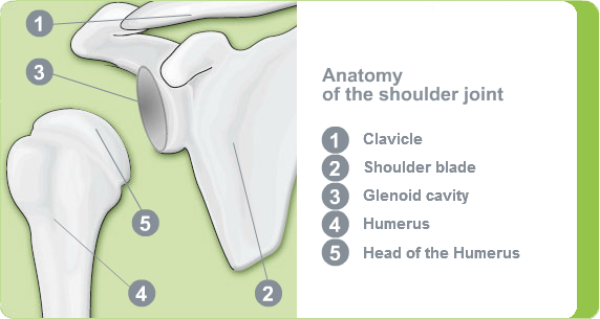
The shoulder joint consists of the following bone structures:
- the head of the humerus: spherical end of the humerus
- the glenoid cavity: shallow concave surface on the shoulder blade
- the acromioclavicular joint: connection to the clavicle
When in a healthy condition, both joint surfaces are covered with a layer of joint cartilage, that acts as a shock absorber, distributes and reduces the forces acting on the shoulder joint. The synovial fluid is a gel-like substance that lubricates the joint and enables a smooth movement of the joint and reduces friction. The shoulder is the most mobile joint in the human body, and is therefore referred to as a primarily muscle.
Role of the Joint Capsule and Rotator Cuff
The shoulder joint is surrounded by a fixed joint capsule, which seals it off from the surrounding tissue. This produces ‘synovial fluid’, which enables the shoulder joint to move free from friction and also supplies the cartilage with nutrients.
Stability and Movement Thanks to Muscles
The spherical head of the humerus is only held very loosely in the small, shallow glenoid cavity of the shoulder blade. For this reason, muscles tendons and ligaments play an important role in stabilising the shoulder joint, while keeping it as mobile as possible. This is mainly achieved by a complex group of muscles known as the rotator cuff. This consists of four muscles which surround the shoulder joint like a cuff, protect it and enable the arm to move. Another important muscle here is the bicep. In addition to the muscles, tendons and ligaments also support the range of movement.
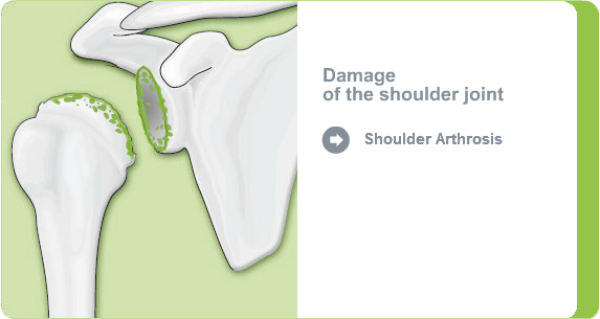
Damage of the Shoulder Joint - How Can the Shoulder Joint Become Damaged?
In order for the shoulder joint to move smoothly and free from pain, the covering of cartilage on the head of the humerus and the glenoid cavity must be intact. Various factors can cause the protective layer of cartilage to become worn or damaged, this is referred to as shoulder arthrosis (omarthritis):
- Damage to the rotator cuff
- Frequent dislocations (luxations)
- Incorrectly loading or overloading of the shoulder joint during work or sport
- Joint inflammation (chronic arthritis, rheumatism)
- Fractures of the humeral head with circulatory problems
In a healthy shoulder joint, the joint cartilage forms a smooth surface, which protects the joint surfaces against friction. In the case of shoulder arthrosis, however, the joint cartilage initially loses its elasticity although the sufferer is unaware of this. The surface of the cartilage becomes rough in the areas subject to the greatest loads and, over time, is completely worn away. The bony surfaces of the joint now rub against each other which can ultimately lead to deformation of the humeral head and glenoid cavity.
Pain and Restricted Movement
If the joint surfaces rub against each other without the protective layer of cartilage, the person affected experiences pain. At first, the patient only experiences pain when the joint is under stress, but, over time, increasingly also when at rest, above all at night. Patients often complain of sensitivity to cold and scraping and rubbing inside the shoulder. The shoulder joint also increasingly loses mobility, ultimately becoming completely stiff. As a result of this, patients adopt a protective posture, which in turn causes muscle tension and pain in other regions of the body, such as the neck or back. As the shoulder joint plays a key role – particularly in everyday activities like lifting and carrying – patients become increasingly restricted in their day-to-day lives and their quality of life can suffer. Even putting on and taking off a jacket, pouring a drink or cleaning your teeth can become a problem.
Pain Relief Options
Depending on the nature of the pain experienced, the attending doctor may explore conservative methods for reducing the pain. These include pain relief and anti-inflammatory medications, physiotherapy, baths and packs. Injections into the shoulder joint can also provide relief. These can help to reduce pain and improve mobility in the joint. Shoulder arthroscopy with irrigation of the joint cavity can also be performed.
However, there are currently no guaranteed methods for healing arthrosis permanently. If all conservative methods have been exhausted, joint-replacement surgery should be performed.
Artificial Shoulder Joint - How Does it Work?
The artificial prosthesis components are made of different materials:
- metal alloys: (titanium, cobalt-chromium, stainless steel)
- special plastic (polyethylene) which replicate the joint cartilage
The surgeon decides which materials to use based on the anatomy, bone condition and age of the patient.
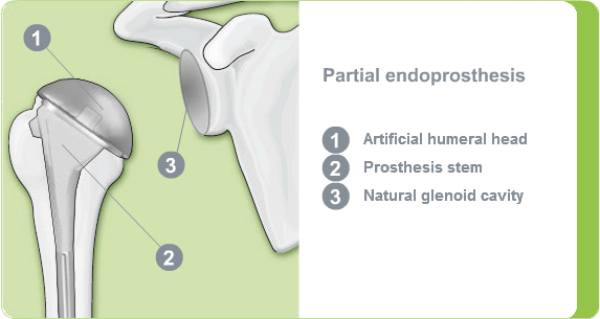
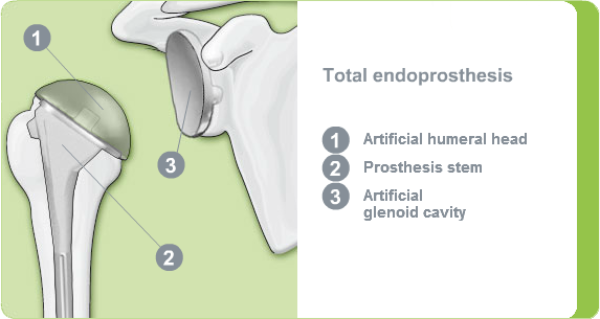
Types of Prosthesis
As the shoulder is a primarily muscle-guided joint, it is important that the surgery is performed in such a way as to protect the soft tissues, muscles, tendons and ligaments as far as possible.
Depending on the condition, age and bone condition of the patient, the following types of prosthesis can be used: partial replacement, total replacement and reverse and cap prosthesis or resurfacing.
With this method, only the damaged joint surface at the head of humerus is replaced, with the addition of a metallic crown. This is referred to as shoulder cap prosthesis.
The prosthesis therefore consists of a cap for the natural humeral head, making this the most minimal form of shoulder joint replacement.
The advantage of this method is that it preserves the bone material of the humeral head, the surgical intervention is relatively small, and blood loss is kept to a minimum. The cap prosthesis does, however, require a sufficiently large contact area, as well as a stable bone condition. This means it is not suitable for osteoporosis patients, for example.
Fixation Artificial Shoulder Joint - How is the Shoulder Endoprosthesis Fixated?
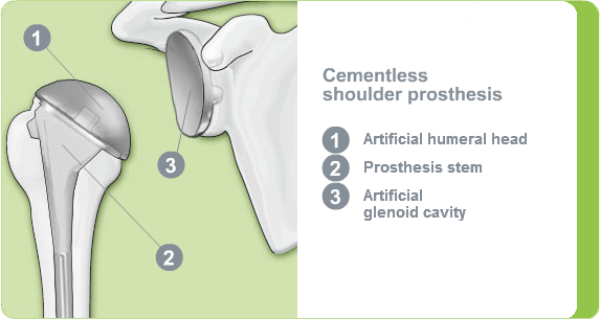
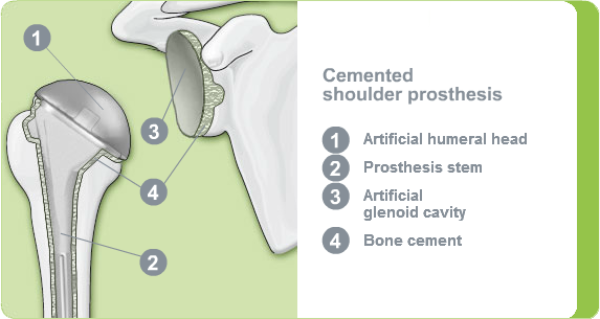
An artificial shoulder joint can be fixated in various ways. In essence, there are two main types of fixation: cemented and cementless:
- In older patients or those with an unstable bone structure, the joint replacement is fixated using bone cement. This creates a strong bond between the shoulder endoprosthesis and the bone immediately after the surgery.
- If the bone quality is good, the shoulder joint can be secured without using cement. With this method, the bone slowly grows into the shoulder prosthesis and only forms a strong connection after some time.
This means selecting the right procedure not only depends on the age of the patient, but also on the condition of the bone. The surgeon decides on the appropriate method with the patient during a preoperative consultation.
In many cases, minimally invasive shoulder surgery, known as shoulder arthroscopy, is performed. This reduces any stay in hospital significantly or eliminates the need for it altogether.
Mobilising the shoulder quickly is crucial for the healing process. Physiotherapy exercises are introduced soon after surgery. Active participation in these exercises is the only way to restore mobility to your shoulder. A lack of movement can lead to adhesions or fusions, which result in restricted mobility or pain.
This method involves fixating the artificial joint with bone cement.
In most cases it is advisable to use bone cement when implanting a shoulder replacement. The slow bone in-growth of the artificial shoulder joint is avoided and the patient can apply load to their arm again immediately following surgery.
What Happens Before Surgery?
Patient Assessment – Your Personal Medical History
In the initial consultation the doctor will ask you about your complaints. They will ask where you have pain and where this pain radiates to. They will also enquire about the intensity of the pain, how long it lasts and any influencing factors which exacerbate or ease the pain.
Physical Examination – Where Does it Hurt?
The doctor will first examine your shoulders, neck, back and both arms and palpate the various structures. They will then conduct some movement tests to gain an impression of the mobility of the shoulder joint. They will also check the level of pain caused by various movements in the shoulder joint, such as adduction, abduction, rotating and raising.
X-ray – Focus on Your Shoulder
Using an X-ray image, the doctor is able to identify changes caused by shoulder arthrosis: i.e. owing to a loss of cartilage the intra-articular space between the humeral head and the glenoid cavity is either no longer uniform, is narrower or is even no longer visible. The bone structure of the humeral head and glenoid cavity appears irregular and altered; in very advanced stages the sections of the joint are deformed.
Preoperative Discussion – Your Chance to Ask any Questions
On the day before surgery, the surgeon will usually talk to you in detail about the planned procedure. During the consultation, they will explain the method of surgery and the type of prosthesis that will be used. Selecting the right prosthesis model depends on your individual bone condition, your body weight and your physical activity. The surgeon therefore normally decides beforehand which prosthesis model and type of fixation to use based on your X-ray and data.
In most cases, the surgeon will ask you about your state of health on the day before surgery. Do not hesitate to inform your doctor of any minor complaints you may have, such as colds and skin infections, even if you are not asked. Although harmless, these illnesses need to be cured before a surgical intervention.
The anaesthetist will also talk to you on the day before the surgery to explain the potential risks involved with the anaesthesia. They will also perform a few minor examinations, with a particular focus on heart and lung function and any possible allergies. They will then discuss the type of anaesthesia to be used.